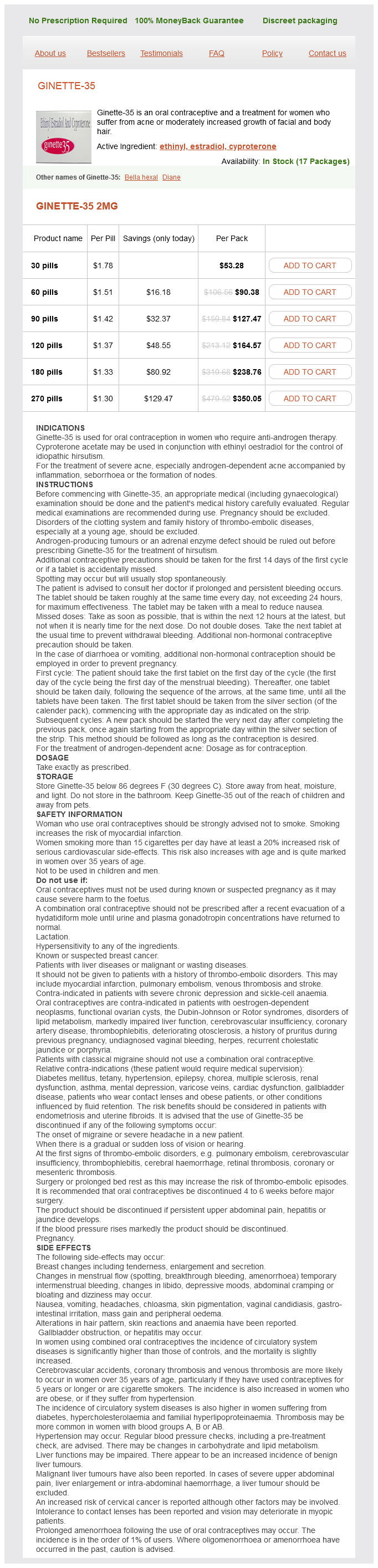
Ginette-35 dosages: 2 mg
Ginette-35 packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills
Only $1.38 per item
In stock: 649
Description
The available data are sufficient to conclude that the combination of pyridoxine and doxylamine is safe and effective for nausea and vomiting of pregnancy women's health clinic balcatta 2 mg ginette-35 buy with amex. Severe deficiency or abnormal metabolism is related to fetal and infantile convulsions and possibly to other conditions breast cancer 2a prognosis 2 mg ginette-35 buy overnight delivery. However, the association of pyridoxine deficiency, with or without folate deficiency, and oral clefts requires confirmation. Like other B-complex vitamins, concentrations of pyridoxine in the fetus and newborn are higher than in the mother and are directly proportional to maternal intake (5Â16). Actual pyridoxine levels vary from report to report because of the nutritional status of the populations studied and the microbiologic assays used, but usually indicate an approximate newborn:maternal ratio of 2:1 with levels ranging from 22 to 87 ng/mL for newborns and 13Â51 ng/mL for mothers (4,14Â16). Pyridoxine deficiency without clinical symptoms is common during pregnancy (10,16Â34). Clinical symptoms consisting of oral lesions have been reported, however, in severe B 6 deficiency (35). Supplementation with multivitamin products reduces, but does not always eliminate, the incidence of pyridoxine hypovitaminemia (16). A brief report in 1976 described an anencephalic fetus resulting from a woman treated with high doses of pyridoxine and other vitamins and nutrients for psychiatric reasons, but the relationship between the defect and the vitamins is unknown (38). The effects on the mother and fetus resulting from pyridoxine deficiency or excess are controversial. In another study, 410 women treated with 10 mg of pyridoxine daily were compared with 410 controls (40). The difference between the mean levels of the two groups, 25 and 33 ng/mL, respectively, was not significant. All were placed on a diet and given 100 mg of pyridoxine per day for 14 days, after which only two were diagnosed as having gestational diabetes mellitus. Other investigators duplicated these results in 13 women using the same dose of pyridoxine but without mentioning any dietary manipulation and without controls (45). Moreover, all of the mothers had large-for-gestational-age infants, an expected complication of diabetic pregnancies. Infantile Convulsions An association between pyridoxine and infantile convulsions was first described in the mid-1950s (48Â52). Some infants fed a diet deficient in this vitamin developed intractable seizures that responded only to pyridoxine. A 1967 publication reviewed this complication in infants and differentiated between the states of pyridoxine deficiency and dependency (53). As noted earlier, pyridoxine deficiency is common during pregnancy, even in well-nourished women, but the fetus accumulates the vitamin, although at lower levels, even in the face of maternal hypovitaminemia. Reports of seizures in newborn infants delivered from mothers with pyridoxine deficiency have not been located. On the other hand, high doses of pyridoxine early in gestation in one patient were suspected of altering the normal metabolism of pyridoxine, leading to intractable convulsions in the newborn (54).
Syndromes
- Breast cancer
- Bubonic plague -- an infection of the lymph nodes
- Antiseptics
- Enlarged bladder
- Joints that are fixed in a contracted position (late in the disease)
- Abnormal reflexes or increased normal reflex responses
- Contact your doctor if you have a cold, flu, fever, herpes breakout, or any other illness.
- Gastroparesis
- Seizures
- Lack of desire to do anything
Placental passage in humans has apparently not been studied pregnancy vs pms purchase 2 mg ginette-35 fast delivery, but the molecular weight (about 384) suggests that the drug will cross to the embryo fetus womens health 012013 pl purchase ginette-35 2 mg overnight delivery. Moreover, the drug is distributed into many human tissues, including the endometrium, fallopian tubes, and ovaries (1). The woman went into premature labor 1 month after completion of the therapy and delivered a baby without evidence of infection or abnormalities (no other details were provided) (2). She responded well to the therapy and was then given amoxicillin (750 mg/day) for 4 weeks. A 2012 case report described the use of meropenem (3 g/day) for 7 days starting on postpartum day 6 by a mother exclusively breastfeeding her infant (4). In another case, a mother breastfed her infant until the 4th postpartum month (5). At 2 months, the mother was treated with a 2-week course of meropenem and tobramycin (doses not specified) for a cystic fibrosis exacerbation. In the above cases, the absence of toxic effects in the nursing infants, even with prolonged therapy, suggests that use of meropenem during breastfeeding is probably compatible. However, additional data are warranted and, until such data are available, infants should be monitored for the most common (2%) adverse effects observed in adult patients (headache, nausea, constipation, diarrhea, anemia, vomiting, and rash (1)). As cited in Meropenem-National Library of Medicine LactMed database, November 6, 2013. No teratogenic effects due to mesalamine have been described and, although toxicity in the fetus has been reported in one case, a causal relationship between the drug and the outcome is controversial. It also results from metabolism in the large intestine of the oral preparation sulfasalazine, which is split to mesalamine and sulfapyridine, and from balsalazide and olsalazine, oral formulations that are metabolized in the colon to mesalamine. The history, pharmacology, and pharmacokinetics of mesalamine and olsalazine were extensively reviewed in a 1992 reference (1). Reproduction studies in rats and rabbits at oral doses of 480 mg/kg/day observed no fetal toxicity or teratogenicity (2). Sulfasalazine and one of the metabolites, sulfapyridine, readily cross the placenta and could displace bilirubin from albumin if the concentrations were great enough. Mesalamine is bound to different sites on albumin than bilirubin and, thus, has no bilirubin-displacing ability (3). Moreover, only small amounts of mesalamine are absorbed from the cecum and colon into the systemic circulation, and most of this is rapidly excreted in the urine (4). The drug and metabolite levels (all in mcg/mL) and the number of patients were as follows: amniotic fluid (N = 4), 0.
Specifications/Details
Turkey Grass (Verbena). Ginette-35.
- How does Verbena work?
- What other names is Verbena known by?
- Treating sinusitis when taken as a combination product containing gentian root, elderflower, cowslip flower, and sorrel.
- What is Verbena?
- Are there safety concerns?
- Dosing considerations for Verbena.
- Sore throat, asthma, whooping cough, chest pain, abscesses, burns, colds, arthritis, itching, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96132
The investigators speculated that pregnant women eating the meat of methimazole-exposed cattle would expose their fetuses to the drug (48) womens health institute of illinois purchase 2 mg ginette-35 with amex. Only two goiters have been reported in carbimazole-exposed newborns and none with methimazole (13) breast cancer awareness facts 2 mg ginette-35 for sale. Long-term follow-up of 25 children exposed in utero to carbimazole showed normal growth and development (15). Combination therapy with thyroidÂantithyroid drugs was advocated at one time but is now considered inappropriate (see also Propylthiouracil) (22,25,47,49,50). Two reasons contributed to this change: (a) use of thyroid hormones may require higher doses of the antithyroid drug to be used, and (b) placental transfer of levothyroxine and liothyronine is minimal and not sufficient to reverse fetal hypothyroidism (see also Levothyroxine and Liothyronine) (24). A 2002 review of the fetal effects of antithyroid drugs concluded that the evidence for a specific methimazole syndrome is inadequate (51). However, the cluster of case reports of aplasia cutis congenita cases suggests a weak association but additional studies are required. A 2007 case report described a male child whose mother had taken methimazole throughout most of pregnancy; 50 mg/day from conception to 5. Examination at 19 months of age revealed the following: height 75 cm (3rd percentile), weight 8. Relevant features included upward slanted palpebral fissures, arched flared eyebrows, small nose with broad nasal bridge, restriction of supinationÂrotation in both arms, and bilateral radioulnar synostosis. In a patient given 10 mg of radiolabeled carbimazole (converted in vivo to methimazole), the milk:plasma ratio was a fairly constant 1. Extrapolation of these results to a daily dose of 20 mg indicated that approximately 3 mg/day would be excreted into the milk (55). Five lactating women were given 40 mg of carbimazole, producing a mean milk:plasma ratio at 1 hour of 0. A new radioimmunoassay was used to measure methimazole milk levels after a single 40-mg oral dose in four lactating women. A 1987 publication described the results of carbimazole therapy in a woman breastfeeding twins (57). The mean free methimazole concentration in milk, determined between 2 and 16 weeks of therapy, was 43 ng/mL (range 0Â92 ng/mL). Mean plasma levels in the twins were 45 ng/mL (range 0Â 105 ng/mL) and 52 ng/mL (range 0Â156 ng/mL), with the highest concentrations occurring while the mother was taking 30 mg/day. No evidence of thyroid suppression was found clinically or after thyroid function tests in the nursing twins (57). Two other studies also found no effect on clinical status or thyroid function in nursing infants of mothers taking carbimazole or methimazole (58,59). In one report, no adverse effects were observed during a 3-week study of 11 infants whose mothers were taking carbimazole 5Â15 mg/day (58). In the other study, normal thyroid function in 35 nursing infants, whose mothers were taking methimazole, was documented over periods ranging from 1 to 6 months (59).
Related Products
Usage: q.3h.
The mother was also taking an antiemetic medication (Bendectin) on an "as needed" basis womens health 3 month workout plan 2 mg ginette-35 purchase with mastercard. In this same report women's health during pregnancy discount ginette-35 2 mg on line, the authors, from data obtained from the Michigan Medicaid program between 1980 and 1983, cited 1020 other cases in which metronidazole use in the 1st trimester for treatment of vaginitis was not linked with birth defects. In an additional 63 cases, use of the agent for this indication was linked to a birth defect diagnosis. In a continuation of the study cited immediately above, 229,101 completed pregnancies of Michigan Medicaid recipients were evaluated between 1985 and 1992 (F. Of this group, 2445 newborns had been exposed to metronidazole during the 1st trimester. Specific data were available for six defect categories, including (observed/expected) 23/24 cardiovascular defects, 1/1 spina bifida, 4/7 polydactyly, 2/4 limb reduction defects, 7/6 hypospadias, and 8/4 oral clefts. Using data from the Tennessee Medicaid program, pregnancy outcomes of women (N = 1307) who had filled a prescription for metronidazole between 30 days before and 120 days after the onset of their last normal menstrual period were compared with those of women who had not filled such a prescription (32). Data were available for 1322 exposed (1318 live births; 4 stillbirths) and 1328 nonexposed (1320 live births; 8 stillbirths) infants. Similar results were obtained when congenital malformations were analyzed by specific types, including those of the central nervous system, heart, gastrointestinal tract, musculoskeletal system, urogenital system, respiratory tract, chromosomal, and by multiple organ systems. The investigators concluded that the use of metronidazole was not associated with an increased risk for birth defects (32). A study published in 1995 conducted a meta-analysis of seven studies (from a total of 32 references identified in their search) that met their criteria for assessing the safety of metronidazole use in human pregnancy (33). The criteria required exposure during the 1st trimester and comparison of these outcomes with the outcomes of pregnancies that were not exposed or only exposed during the 3rd trimester. Based on these findings, the investigators concluded that the use of metronidazole during the 1st trimester was not associated with an increased risk of congenital defects (33). A second meta-analysis, similar in design to the study above, evaluated the risk for birth defects after the use of metronidazole early in pregnancy (34). A total of five studies, one unpublished caseÂcontrol study and four published cohort studies, met the inclusion criteria. A large ethnically homogeneous population-based dataset (Hungarian Case Control Surveillance of Congenital Abnormalities, 1980Â1991) was used in a study published in 1998 to evaluate whether the use of metronidazole in the 1st trimester was associated with congenital anomalies (35). Minor abnormalities and congenital abnormality syndromes of known origin were excluded. The investigators concluded that the most likely reasons for the association were recall bias or chance alone, but that a true association could not be ruled out. However, based on the prevalence of isolated cleft lip (with or without cleft palate) in their population and the prevalence of exposure to metronidazole during the 2nd and 3rd months of pregnancy, their analysis suggested that even a true association would only increase the prevalence of the defect from 100 cases/100,000 births to 103 cases/100,000 births. Moreover, the finding was not confirmed when the comparison was made with the total control group (35). In a second study from the above group, the teratogenic potential of vaginal metronidazole plus miconazole treatment during the 2nd and 3rd months of pregnancy was evaluated using the 1980Â1996 dataset of the Hungarian Case Control Surveillance of Congenital Abnormalities (36).
Additional information:
10 of 10
Votes: 134 votes
Total customer reviews: 134
Tags: order ginette-35 2 mg with amex, buy 2 mg ginette-35 with visa, order ginette-35 2 mg free shipping, purchase ginette-35 2 mg mastercard, ginette-35 2 mg with amex, generic 2 mg ginette-35 free shipping, purchase ginette-35 2 mg overnight delivery, buy ginette-35 2 mg overnight delivery
Customer Reviews
Luca, 26 years: In addition, acute heart failure occurred during the first 3 days after birth (5). The animal reproduction data suggest a potential for toxicity, but not for teratogenicity.
Hamil, 22 years: The molecular weight (about 293) and the moderate elimination half-life suggest that the drug will cross to the embryoÂfetus, but the extensive metabolism may limit the amount of parent drug crossing the placenta. Based on the above data, naloxone should not be given to the mother just before delivery to reverse the effects of narcotics in the fetus or newborn unless narcotic toxicity is evident.
Achmed, 46 years: Effects of ranitidine on maternal gastric juice and neonates, when administered prior to caesarean section. However, one investigator concluded in 1977 that lipid infusions were contraindicated during pregnancy for several reasons: (a) an excessive increase in serum triglycerides, often with ketonemia, would result because of the physiologic hyperlipemia present during pregnancy; (b) premature labor would occur; and (c) placental infarctions would occur from fat deposits and cause placental insufficiency (15).
Folleck, 24 years: Although the incidence is unknown, the rare reports of this toxicity combined with the popularity of the drug for urinary tract infections in pregnant women suggest that the risk is rare. Panitumumab may cause severe, infusion-related toxicity, including hypotension and other adverse effects.
Hamlar, 50 years: The mechanism for this interaction may involve the interruption of the enterohepatic circulation of contraceptive steroids by inhibiting gut hydrolysis of steroid conjugates, resulting in lower concentrations of circulating steroids. At this dose in both species, serum levels in fetal animals at delivery were approximately 35% of maternal levels.
Potros, 48 years: The American Academy of Pediatrics classifies nifedipine as compatible with breastfeeding (18). The use of pamidronate is not recommended in women who may become pregnant or during pregnancy.
Angir, 65 years: More than 100 compounds have been isolated from peppermint oil, but the primary pharmacologically active agents are menthol (29%Â48%), menthone (20%Â31%), and menthyl acetate (3%Â10%), and lesser amounts of caffeic acid, flavonoids, and tannins (2). A 2005 review of acromegaly pharmacotherapy stated that pegvisomant should not be used in pregnancy (4).
Kaffu, 28 years: Moreover, a significant increase in loratadine-induced congenital malformations would be unusual, as no other antihistamine has been shown to be a major human teratogen. Three (23%) of the methylergonovine group failed to conceive or resorbed their conception compared with an average of 17% (10 of 58) in the other three treated groups and 17% (2 of 12) in the controls.